You have no items in your shopping cart.
Fibrinogen and Fibrin: Central Components of Hemostasis and Inflammatory Regulation
Exploring the dual role of liver-derived glycoproteins in coagulation and host defense.
Fibrinogen and its activated form, fibrin, are essential plasma glycoproteins. Synthesized in the liver, they serve as the backbone of blood coagulation, maintaining vascular integrity and orchestrating the body’s innate immune response.
I. Molecular Characteristics
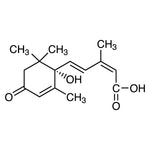
Fibrinogen is a large, hexameric glycoprotein consisting of three pairs of polypeptide chains: Aα, Bβ, and γ. These chains are intricately linked by disulfide bonds, maintaining a soluble, inactive state under normal physiological conditions.
II. The Coagulation Cascade: Conversion to Fibrin
Upon vascular injury, the cascade triggers Thrombin generation, which acts as the molecular "switch":
- ✔ Enzymatic Cleavage: Thrombin removes fibrinopeptides A and B.
- ✔ Polymerization: Fibrin monomers spontaneously assemble into insoluble fibers.
- ✔ Stabilization: A 3D meshwork forms, sealing the wound and preventing blood loss.
III. Host Defense and Inflammation
1. Immune Enhancement
Fibrin matrices act as scaffolds, enhancing the recruitment and phagocytic efficiency of immune cells at the site of infection.
2. Acute Phase Response
During trauma or infection, fibrinogen levels surge to modulate cytokine production and limit systemic tissue damage.
3. Barrier Formation
The fibrin deposit creates a physical barrier that restricts pathogen spread while guiding tissue repair and cell migration.
IV. Pathophysiological Implications
While essential, dysregulated fibrinogen elevation is a known risk factor for thrombosis. Excessive fibrin formation can lead to pathological clots, vascular occlusion, and chronic inflammatory complications. Balancing these levels is critical for vascular health.